Research in the Guertin Lab at UMass Chan Medical School
We study the biology of nutrient sensing. One of the most basic requirements for an organism to survive and thrive is having the ability to sense food and respond to changes in nutrient availability. Our main objective is to elucidate biochemical mechanisms of nutrient sensing and their significance to the pathogenesis of metabolic diseases, including type 2 diabetes and cancer. We are specifically researching how signal transduction pathways and the metabolic machinery intersect, focusing on the insulin and mTOR pathways. We also study the biology of brown and white adipose tissues and how adipose tissues sense nutrient availability, store, release, and consume nutrients, and communicate with other organs to maintain energy balance. Our long-term goal is to identify key nodes of metabolic control that can be targeted therapeutically to improve human health.
Signaling
Signaling pathways and metabolic pathways have historically been studied separately, but we now know they are intimately linked. For example, circulating growth factors through cell surface receptors activate intracellular signaling networks, which promote the uptake and metabolism of nutrients. Inside the cell, the products of metabolism (called metabolites) also function as second messengers that regulate signaling pathways and gene expression. These connections are often altered in type 2 diabetes (T2D) and cancer. One aim of our lab is to understand how diverse cells sense and respond to nutritional cues by defining critical points of intersection between signaling and metabolism. Learn More
Metabolism
Another goal of our research is to understand how modifiable and non-modifiable risk factors including over-nutrition and mutations cause metabolic diseases such as T2D and cancer. The greatest risk factor today for type 2 diabetes is being overweight or obese, and there is mounting evidence that obesity promotes cancer. In fact, obesity will soon overtake smoking as a leading cause of death in the US. The obesity epidemic has also brought adipose tissue, and its cellular unit - the adipocyte - to the research forefront in understanding and fighting this serious global challenge. We are interested in how different food sources impact adipose tissue function and crosstalk and how metabolic health impacts other diseases including cancer and neurodegeneration. Learn More
Adipocytes
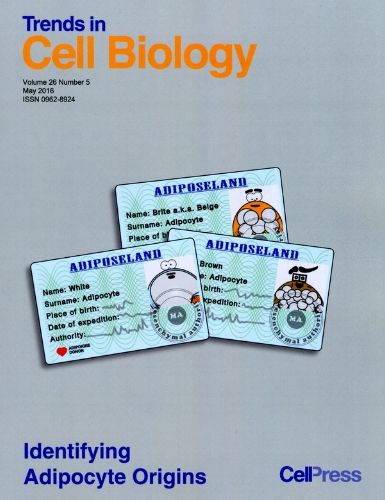
Adipocytes are the body’s major energy storage site, but they also have critical nutrient sensing and endocrine functions. Understanding how adipocytes respond to nutritional and hormonal cues is critical to understanding why obesity causes T2D and cancer. Adipocytes come in different ‘shades’ each with unique metabolic properties. For example, brown adipocytes burn fat to make heat; white adipocytes store and release energy during feast and fasting, respectively; and brite or beige adipocytes can switch between brown and white adipocyte characteristics. However, this an oversimplification as additional subclassifications of adipocytes likely exist. While the obesity epidemic has given fat a bad rap, its development was critical in our evolution, and having healthy adipocytes is essential for our metabolic fitness. We are using a variety of in vivo and in vitro approaches to understand the biology of these fascinating cells. Learn More