Hepatic Vascular Cavernomas
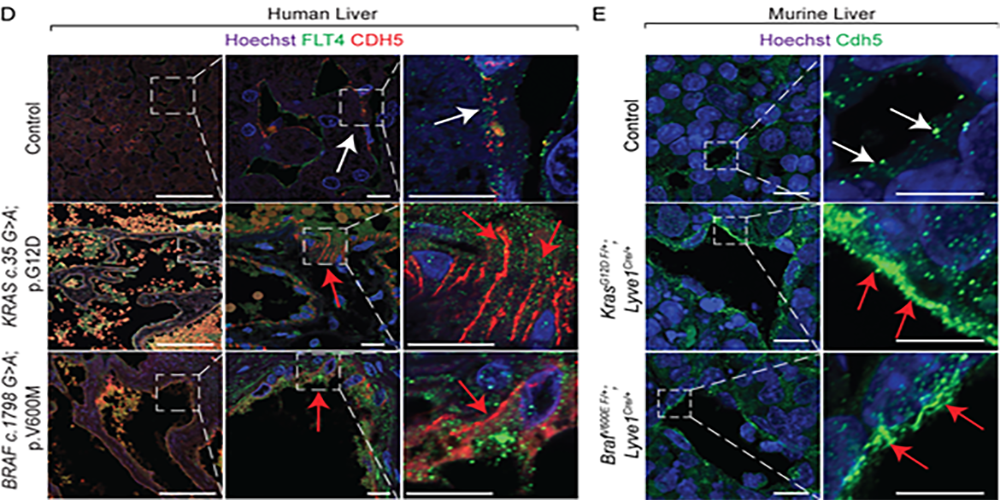
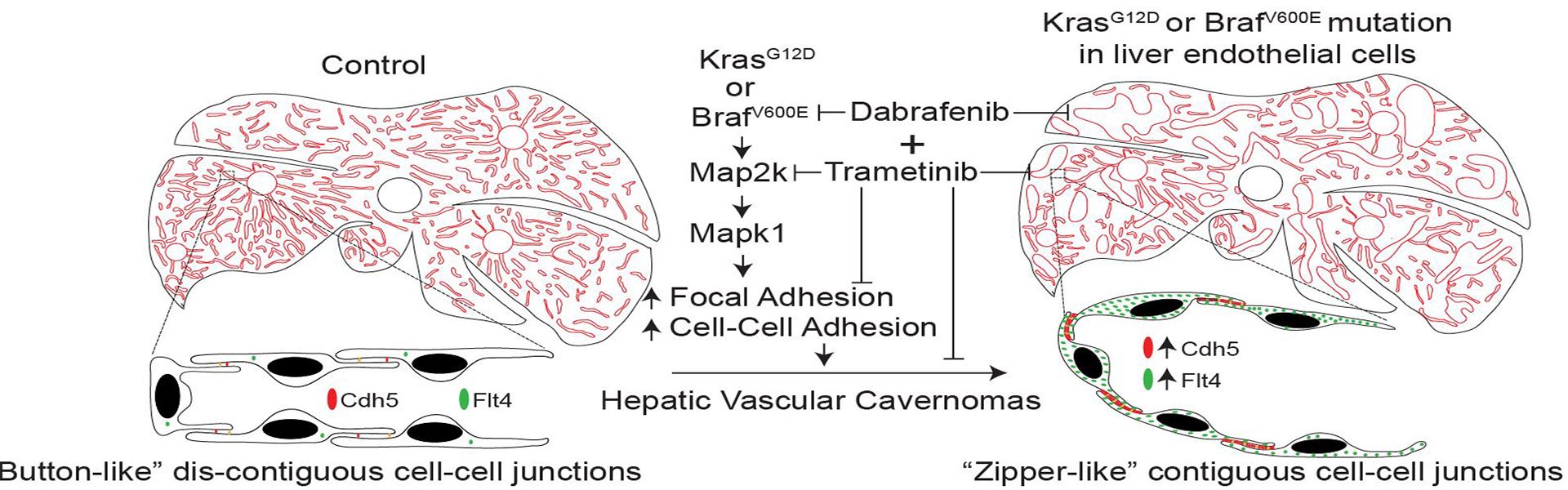
Hepatic vascular cavernomas, the most common benign tumor of the liver, cause lethal complications such as hepatic rupture, consumption coagulopathy, and cardiac failure. Although Virchow and Frerichs described hepatic vascular cavernomas as a distinct clinical entity in the mid-1800s, their genetic etiology, molecular mechanism, and effective treatment remain undefined. Recently we identified gain-of-function mutations in KRAS or BRAF genes within liver endothelial cells as a causal mechanism for hepatic vascular cavernomas (Journal of Experimental Medicine). We identified gain-of-function mutations in KRAS or BRAF genes in pathological liver tissue samples from patients with hepatic vascular cavernomas. Mice expressing this human KRASG12D or BRAFV600E gain-of-function mutations in hepatic endothelial cells recapitulated the human hepatic vascular cavernoma phenotype of dilated sinusoidal capillaries with defective branching patterns. KRASG12D or BRAFV600E induced “zipper-like” contiguous expression of junctional proteins at sinusoidal endothelial cell-cell contacts, switching capillaries from branching to cavernous expansion. Pharmacological or genetic inhibition of the endothelial RAS–MAPK1 signaling pathway rescued hepatic vascular cavernoma formation in endothelial KRASG12D- or BRAFV600E-expressing mice. These results uncover a major cause of hepatic vascular cavernomas and provide a road map for their personalized treatment.