 |
|
|
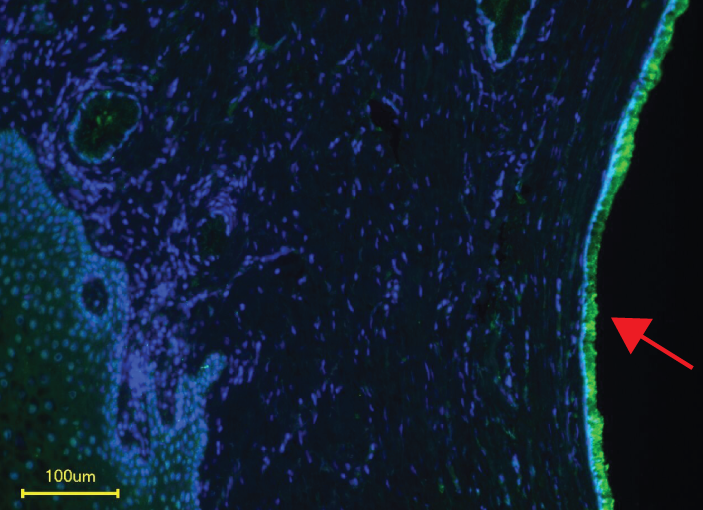
Siglec-11 receptors (red arrow) are expressed on human cervical epithelia, the main infection site of the gonococcus. |
Research from UMass Medical School and the University of California San Diego reveals new insights into how gonococcus, the bacteria that causes gonorrhea, latches onto and enters human cells. The study, published in Evolutionary Applications, suggests new avenues to develop treatments that defend against bacterial infection.
Since reaching a historic low in 2009, the number of cases of gonorrhea in the United States has increased nearly 50 percent to a total of 468,514 in 2016, according to the Centers for Disease Control. A sexually transmitted disease, gonorrhea has also become increasingly resistant to antibiotics. Scientists are engaged in better understanding why the gonorrhea bacterium only affects humans, how the bacterium establishes itself in host cells, and how the body responds, in order to develop new ways to prevent and treat the disease.
“Understanding how bacteria evade our immune system will provide novel ways to target multidrug-resistant pathogens,” said Sanjay Ram, MD, professor of medicine and an author on the new study.
Gram-negative diplococci bacteria, such as gonococcus, are known for “stealing” sialic acid molecules from the cells of human hosts and cloaking itself in them. This disguise is known to help bacteria avoid recognition and bind host Siglecs, a sialic acid-specific receptor found on the surface of human immune cells. The ability to bind Siglecs allows the bacteria to gain a foothold in the human body. When bound by the bacteria, most Siglecs dampen the immune response.
Researchers were surprised to discover, however, that gonococcus doesn’t need its sialic acid coat to bind to Siglecs after all. They learned that the bacterium itself, using a protein called porin (PorB), can also bind multiple human Siglecs on both immune cells and female genital tract cells, including anti-inflammatory Siglec-11 and pro-inflammatory Siglec-16. These findings also suggest that a person’s Siglec variations may influence his or her susceptibility to the infection.
“The sialic acid-Siglec interaction has always been thought of as gonorrhea’s initial ‘handshake’ with its host,” said Ajit Varki, MD, distinguished professor of medicine and cellular & molecular medicine at UC San Diego School of Medicine. “But it seems that over time the bacterium’s own native proteins evolved to directly bind Siglecs themselves, even without sialic acid.”
Dr. Varki, Dr. Ram and colleagues also studied how this interaction between the gonococcus and Siglecs functions in a Namibian community in which 72 percent of sexually active women have gonorrhea, a population studied by co-author Ashley Hazel, PhD, research scientist at Stanford University. By looking at anonymized genomic DNA sequences from 418 women, they found that uninfected women were more likely to have Siglec-14 and Siglec-16 than infected women, suggesting that these immune response-stimulating versions of the receptor provide some protection against the bacteria.
“There are many Siglec variants and your unique arrangement of them may determine how your cells initially interact with the gonococcus, or other microbes, and how your immune system responds to it,” said Varki.
These findings open the possibility that gonorrhea infections might be prevented or treated with an antibody or small-molecule-based drug that inhibits the gonococcus’ interaction with anti-inflammatory Siglecs or boosts pro-inflammatory Siglecs.
Meanwhile, Ram’s team, in collaboration with the Varki group and researchers at the National Research Council, Ottawa, have been trying to out-smart the gonococcus by feeding it false sialic acids, in the hopes of disrupting its ability to bind Siglecs and establish infection.