AHA grant to probe the heart of COVID-19 infections
Aug. 26, 2020
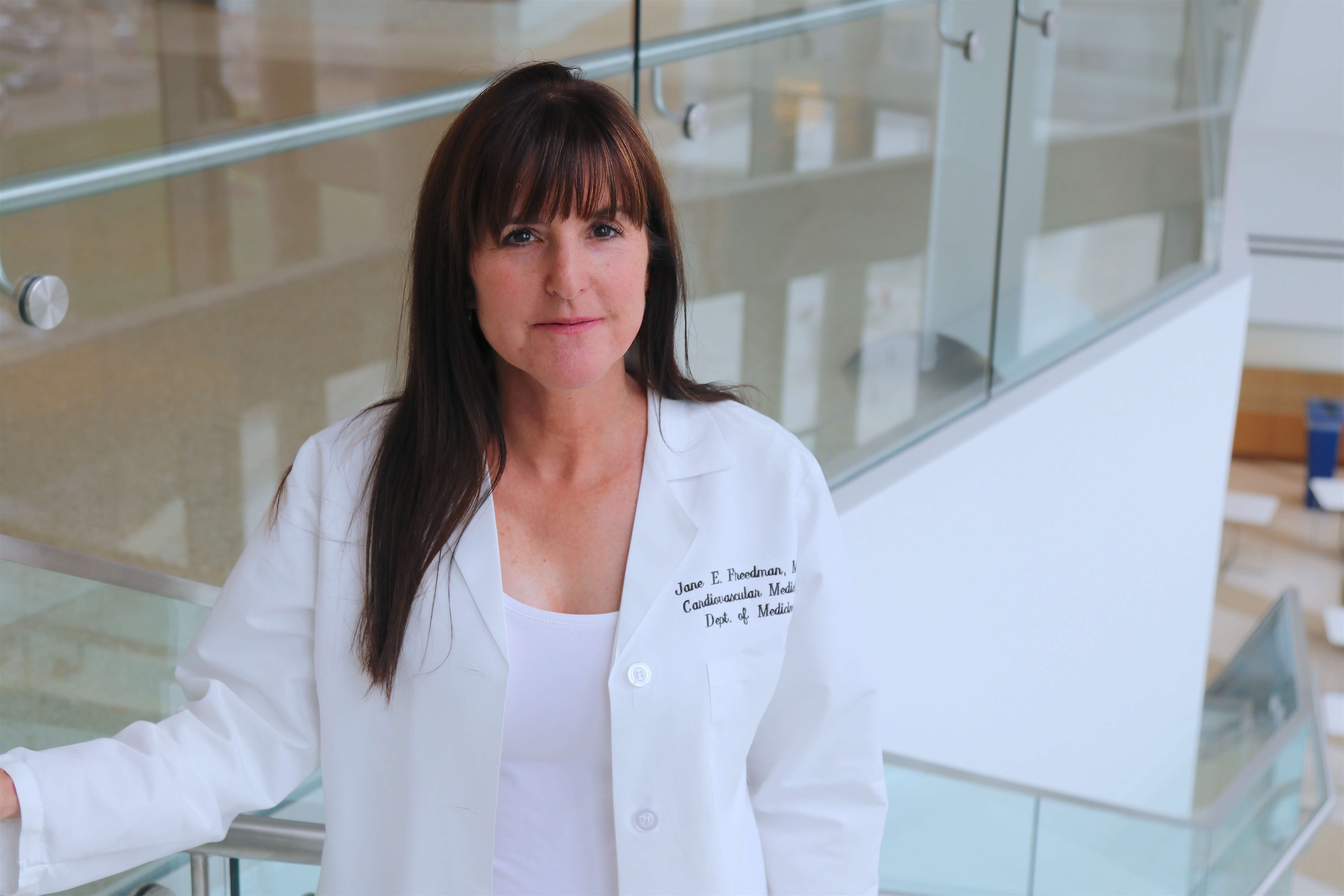
When it became painfully clear that COVID-19 causes significant cardiac disease in many patients, with potentially deadly blood clots appearing in the heart, lungs and other organs, Jane Freedman, MD, had a striking insight.
“We had some findings in our work on influenza and cardiovascular disease that led us to believe our capabilities could be adapted to investigate what was going on with this new coronavirus,” said Dr. Freedman, the Edward Budnitz, MD, Professor in Cardiovascular Medicine and professor of medicine at UMass Chan Medical School, and director of translational research for UMass Memorial Heart and Vascular Center, where she is an attending physician.
The connection between influenza and heart damage wrought by SARS-CoV-2, the virus that causes COVID-19, could be platelets, Freedman theorizes. The American Heart Association (AHA) saw merit in exploring that idea and awarded the Freedman lab a grant to fund the project titled “The Role of the Platelet in Mediating Cardiovascular Disease in SARS-CoV-2 Infection.”
“The American Heart Association is in a unique position to mobilize significant resources very quickly and pivot to provide funding to address this pandemic,” Freedman said. “In a very short time, they had hundreds of experts reviewing COVID-19 related proposals, to better understand the disease and to search for potential clinical interventions. We are fortunate, and thankful, to be funded.”
Freedman’s research explores the genetic and molecular mechanisms that cause the clots that lead to heart attacks and strokes. Much of that work focuses on platelets, which are small cell fragments that circulate in the bloodstream.
Historically, it was understood that the role of platelets was to form clots that stop bleeding. They patrol the circulatory system, and if they find a breech in a blood vessel (from a cut in the skin or other trauma) they stick to the site and release molecules that prompt other platelets to do the same, thus building a clot. Platelets also release signals that attract certain proteins to help close a wound. When platelets malfunction, however, they can build up unchecked in an intact blood vessel and block the flow of blood, causing a heart attack if the clot is in a coronary artery or a stroke if the clot is in the brain.
However, recent discoveries by the Freedman lab and others reveal a more expansive role for platelets as front-line sentinels of the immune system.
It has been documented for years that patients hospitalized with severe influenza are more likely to have a heart attack. The Freedman lab explored that connection by analyzing blood samples from patients hospitalized with severe influenza and found numerous molecular markers that indicated that platelets were attacking the influenza virus. Then, the lab team cultured the flu virus with blood samples from healthy donors and found the platelets in those samples could recognize the flu virus and engulf it.
Those findings suggest that platelets attack the flu virus and set off a cascade of signals that prompt a broader immune response. In some cases, platelets may react too strongly to the flu virus and cause excessive inflammation and clotting that can lead to a heart attack, Freedman said.
“We want to know if platelets are also reacting to the coronavirus, orchestrating the initial immune response,” she continued. “And we want to know if dysregulation of the platelet response can cause inflammation and contribute to cardiovascular disease in COVID-19 patients.”
Jeffrey J. Rade, MD, professor of cardiovascular medicine at UMass Chan and an interventional cardiologist at UMass Memorial, is working with the Freedman lab on the project. Dr. Rade will collect blood samples from hospitalized COVID-19 patients who are also being treated for heart disease. The Freedman lab with the assistance of Milka Koupenova, PhD, an expert in platelet processes, will analyze the samples to look for platelet activity, and to screen for a wide range of genetic and molecular factors.
The work has already started, thanks to the support of the AHA, and the Freedman lab hopes to have data to report in early 2021.
“Philanthropy like this is extremely important,” Freedman said. “We need to move fast on this, and the American Heart Association is willing to take a risk on early studies.”