Mathers Foundation helps battle COVID 19
The virus that causes COVID-19 can’t survive on its own. By its nature, like all viruses, it first needs to hijack a person’s own cellular machinery to replicate itself, spread the infection and cause disease.
Armed with a major new grant from the G. Harold and Leila Y. Mathers Charitable Foundation, a team of researchers at UMass Medical School is seeking to disrupt the virus’s pathway of attack with a two-pronged approach: blocking its genes from replicating and modulating the body’s immune response to the virus, so it doesn’t rage out of control causing the most severe form of the disease.
“This is a project of great merit and we are thankful for the Mathers Foundation’s support,” said Thoru Pederson, PhD, the Vitold Arnett Professor of Cell Biology, professor of biochemistry & molecular pharmacology and associate vice provost for research at UMMS. “When the Mathers Foundation opened a special program for COVID-19 research, the fact that we already had, on campus, a coronavirus research project that they saw as among the best in the country, is something we can be proud of.”
The disease COVID-19 is caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). While the virus can spread throughout the body and infect many different tissues, its first target is usually the airway leading to the lungs. There are several types of cells in the airway and the virus infects some, but not all of those cells.
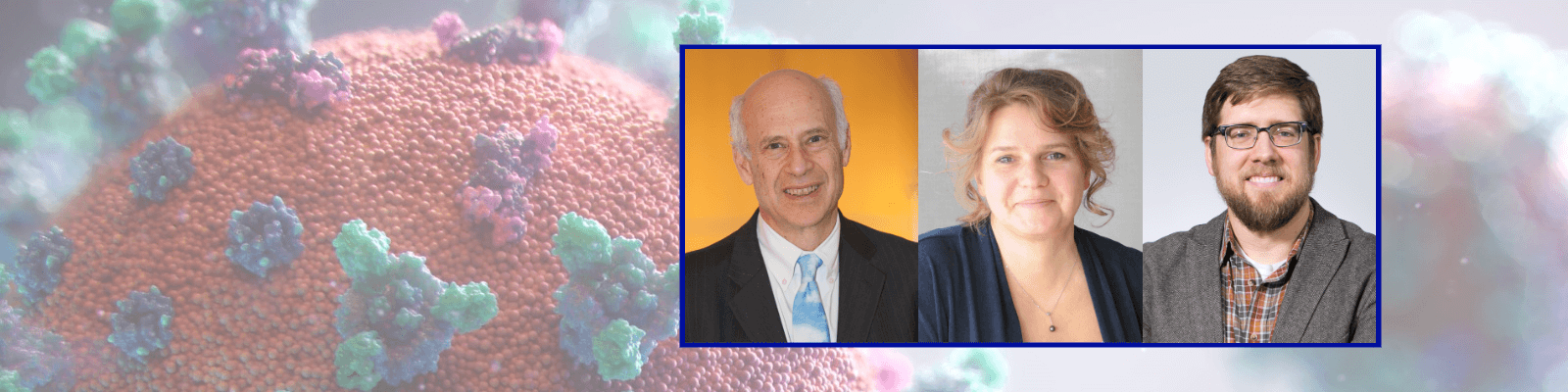
The new grant supports a project led by Robert Finberg, MD, the Richard M. Haidack Professor of Medicine, chair and professor of medicine; Anastasia Khvorova, PhD, the Remondi Family Chair in Biomedical Research, professor of RNA therapeutics; and Jonathan K. Watts, PhD, associate professor of biochemistry & molecular pharmacology. Both Drs. Watts and Khvorova work within the RNA Therapeutics Institute at UMMS. Rounding out the team on this project are William McDougall, PhD, assistant professor of microbiology & physiological systems, and Jennifer Wang, MD, professor of medicine.
The investigators will an analyze which airway cells are infected by SARS-CoV-2, then proceed to determine how specific genes, both in the virus and in the human cells, are involved in the infection and replication processes. They will also examine which genes in the host cells are involved in the immune response to the infection. The most severe cases of COVID-19 disease involve a “cytokine storm,” which means the patient’s immune system reacts so strongly to the virus that it causes collateral damage to healthy tissues.
Dr. Finberg is an expert on the processes of viral infection. For the past three flu seasons, he’s led a research project analyzing samples from people sick with the flu. Finberg and colleagues developed an advanced technology platform to study changes in gene expression of individual cells during the processes of influenza infection and the subsequent immune response.
When the pandemic hit, many UMMS labs turned their research program towards the virus. Finberg launched two clinical trials at UMass Memorial Medical Center testing the impact of two pre-existing drugs—remdesivir and favipiravir—on patients admitted with COVID-19 disease. He also opened a new line of research, applying the technology platform developed to study the flu to the SARS-CoV-2 virus.
In that new project, now funded by the Mathers Foundation, Finberg’s team is collecting samples from COVID-19 patients’ airways to determine which cells are prone to infection, which are not and how those cells react at the genetic level in the presence of the virus. That genetic information, along with data published by others, will be used by Khvorova and Watts to design novel RNA- and DNA-based molecules that can target the viral and host cell genes to treat or prevent COVID-19.
Prior to the pandemic, the Watts and Khvorova labs were working to develop new classes of gene-silencing drugs to treat a range of diseases; they, too, rapidly adapted their work to target SARS-CoV-2. The essence of their ongoing approach is to engineer a stable delivery system that can seek out specific cells and deliver a payload of RNA and/or DNA strands that will silence a disease-causing gene.
Much like a delivery truck can carry a variety of different packages to a specific address and keep them safe from the hazards of traffic and bad weather along the way, the Watts and Khvorova technologies seek to protect their designed RNA and DNA packages from being degraded in the bloodstream, so they arrive at their targets intact. The packages differ depending on the targeted gene, but the protective carrying system is largely the same. So, if their effort succeeds, the approach could be used to treat many diseases.
“The platform technologies we develop in this project have the potential to be applied to future viral pandemics, to be better prepared for the next emerging infectious disease,” the research team wrote in the grant application made to the Mathers Foundation, which is a longtime and generous supporter of UMMS.