In a quest to save their daughter, one couple finds hope at UMass Chan
Dynamic fundraising efforts support promising research to cure rare disease
In August 2013, Christine Waggoner and her husband Douglas Dooley faced every parent’s worst nightmare. Their 5-year-old daughter Iris was diagnosed with GM1 gangliosidosis, a rare, fatal condition that destroys nerve cells in the brain and spinal cord. It’s part of a group of neurodegenerative disorders known as lysosomal storage diseases. GM1 leaves children unable to speak, swallow, see, hear or move their limbs. They all eventually die. There is no cure.
Yet.
Gene therapy research underway at UMass Medical School holds tremendous promise for treating this devastating disease. And thanks to Waggoner’s and Dooley’s fundraising efforts to support this work, achieving that promise may be closer than ever.
Seeking answers after Iris’ diagnosis, Waggoner began utilizing the internet and social media to find other families with children who have GM1. The condition is known to affect only a couple of dozen children a year in the U.S., underscoring how challenging her search was.
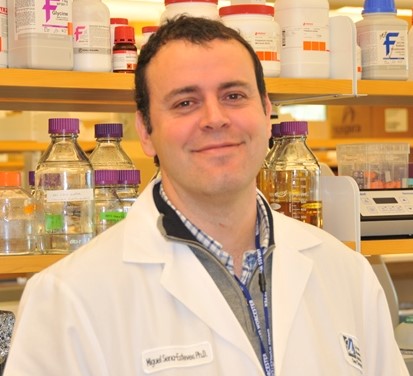
Miguel Sena-Esteves, PhD
“I came across an appeal for funding to complete the IND (investigational new drug application to the FDA) for a clinical trial to study a gene-based therapy for GM1 in humans,” said Waggoner. Soon after, she learned of UMass Medical School’s Miguel Sena-Esteves, PhD, associate professor of neurology, the lead collaborator on groundbreaking gene therapy research for GM1. It gave her family hope that they might be able to save Iris.
In the meantime, Waggoner saw a viral video produced by another family whose child had Sanfilippo syndrome (another lysosomal storage disease); it had raised nearly $2 million in donations.
“I realized we could be doing more for GM1 research,” she said. “Fortunately, my husband and I have a background in media, so we produced a video, too.”
But that wasn’t all. Because Iris loves art, Waggoner organized an art auction that raised $100,000 in a single evening in April 2015, with the funds going directly to Dr. Sena-Esteves’ GM1 gene therapy research. She and Dooley also established a nonprofit foundation and set up a GoFundMe page to accept donations. They built two websites (www.curegm1.org and www.sweetiris.org). They started a Facebook page and a Twitter account. And they continually remind donors to seek matching funds from their employers whenever possible.
By the end of July 2015, they raised upwards of $500,000—most of it within their first four months of fundraising. All monies from those efforts went directly to the Sena-Esteves lab and to the lab of longtime GM1 research collaborator, Douglas T. Martin, PhD, at Auburn University.
“This is an amazing time in medical history with gene therapies being developed. That there may be a chance of dealing with these diseases is amazing.”
In GM1 gangliosidosis, due to a gene mutation, the body produces an insufficient amount of an enzyme called beta-galactosidase. This dysfunction results in cell death, particularly in extremely fragile neurons and spinal cells. As a result, the disease robs children of nearly every skill and bodily function required to live. GM1 is estimated to occur in one in 360,000 newborns.
Sena-Esteves’ lab is investigating new gene-therapy approaches for treating lysosomal storage diseases, including GM1. He and his collaborators have devised new ways to deliver therapeutic levels of the missing enzymes to the entire brain by injecting adeno-associated virus (AAV) vectors into the central nervous system.
“This means we introduce a good version of the mutated gene using a virus as the delivery vehicle,” Sena-Esteves explained. “The virus ‘infects’ the neuron and delivers genetic material that tells the neuron to start making normal proteins. This turns cells inside the patient’s brain into micro-factories that pump out normal enzymes to the other cells that need them.”
Sena-Esteves reports that, in animal studies, this gene therapy has demonstrated a remarkable
increase in lifespan from 8 months to more than 4.5 years, with dramatic improvements in quality of life.
“These experiments have been spectacular,” he said. “It’s so very exciting, and there’s not much else to do now but to test this in patients.”
In fact, in February 2015 UMass Medical School entered into a groundbreaking agreement to collaborate with Lysogene, a French biotechnology company, and Auburn University to develop pre-clinical studies of GM1. The collaboration combines Lysogene’s clinical expertise in gene therapy with the pre-clinical expertise and infrastructure of UMMS and Auburn University.
“We will take one of the gene therapy approaches for GM1 into a first-generation clinical trial in humans,” Sena-Esteves said. “We’re doing the work now to go to the FDA about this.
“Christine’s funding also allows us to expand on other ideas to develop next-generation gene-delivery vehicles, which brings us ever closer to a cure,” he continued. “It shows how one person can have a tremendous impact—and not just on this rare disease; it’s likely that our findings may be translatable to other neurological diseases as well.”
For Waggoner and her family, these advances can’t come too soon.
“I feel a tremendous sense of urgency,” she said. “Iris is 7 years old; it’s around the age of 10 that symptoms become extreme if untreated. If ahuman clinical trial emerges by 2017, we’ll be right on the cusp.
“The reality is that this research is extremely promising,” Waggoner continued. “This is an amazing time in medical history with gene therapies being developed. That there may be a chance of dealing with these diseases is amazing.”
For more information, please visit www.curegm1.org or www.sweetiris.org.