The Story of the MLP: From Clinical Problem to Solution
by: Kevin Houston, OD
My laboratory develops devices and therapies to restore movement of ocular structures paralyzed by stroke and other neuro-pathologies. We have pioneered the use of neodymium and other rare-earth static magnetic materials to provide the force lost due to de-innervation of ocular musculature.
I developed the MLP in response to a clinical need in my practice, providing inpatient low vision rehabilitation care on stroke and brain injury units. I would occasionally encounter patients with recent onset very severe total or near total bilateral blepharoptosis (ptosis), or total ptosis in a better seeing eye. The only available intervention at the time was the ptosis crutch, a wire on the glasses to mechanically prop the lid open first introduced in the 1890’s! Contrivance is often cited as a treatment option, but only rarely used in clinical practice. It has been unacceptable since its introduction because it does not allow the eye to close and could injure the eye if there were a fall. More commonly I would encounter these patients with one eye taped open leading to secondary problems of ocular surface desiccation and lid skin irritation.
The first human subjects’ clinical trial of the MLP was funded by the Massachusetts Lions Eye Research Fund and an NIH K-12 award. It was conducted on the inpatient stroke and brain injury units at Spaulding Rehabilitation Hospital in Charlestown, MA, and found good safety and efficacy for 2 hours per day use and superiority over the ptosis crutch. A second pilot study in outpatients was funded by a Research to Prevent Blindness Grant and resulted in successful use in six patients while defining areas for improvement.
Following the success of the initial clinical trials, the National Institutes of Health (NIH) funded a $2.3m R01 project and a $500K phase I SBIR to advance the technology and test it for longer-term management, which included patients with neuro-muscular causes such as Myasthenia Gravis and Chronic Progressive External Ophthalmoplegia. The most common method currently used to address chronic severe ptosis involves surgically connecting the eyelid to the forehead muscles via a sling (made of silicone or autologous fascia), allowing the patient to lift the lid by raising the eyebrow. In such cases the surgeon will not fully correct the ptosis, in order to avoid overcorrection, which can have dire consequences of exposure leading to desiccation and eventually ulceration of the cornea.
The value of an MLP device most impacts the nearly 80,000 ptosis patients seeking care in the U.S. who are less than ideal surgical candidates, providing them with a fast, non-surgical, and cost-effective alternative. Patients with severe ptosis and their surgeons will no longer have to worry about discomfort and over-correction associated with current treatments risking their long-term ocular health. Additionally, the fit and strength of the MLP device can be easily adjusted at any time as symptoms may change, providing the best comfort and peace of mind. To receive a link for viewing a video of the device on patients with severe ptosis, please contact kevin.houston@umassmed.edu
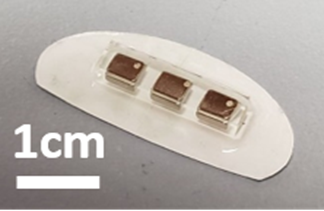
![]()
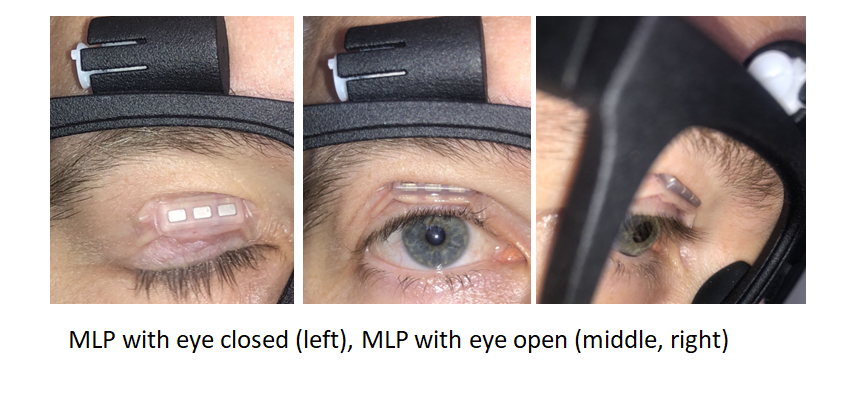

1. Motorized MLP for Total Facial and Eyelid Paralysis: Dr. Houston and his team have built and patented a motorized MLP device that has shown promise to fully automate blinking for patients with total facial and eyelid paralysis. There is currently no treatment option for this rare but devastating condition which typically results in corneal scarring and can lead to blindness due to chronic exposure.
2. Magnetic Re-Animation of Eye Movement: Similar concepts developed to move the eyelid may be able to move the eye when there is paralysis of one or more eye muscles. This problem occurs in 10-20% of stroke survivors and is also common after severe head trauma and neuromuscular disorders. There is no good solution for these patients. Some may be candidates for surgical procedures to partially restore eye movement by translating an intact muscle to the paretic side of the globe. When paralysis is severe, there is no acceptable treatment option and patients often must wear an eye patch indefinitely.
|
Exhibit A |
Exhibit B |
Exhibit C |
Exhibit D |
|
A) Prototype motorized system for fully automated blinking in total facial and eyelid paralysis. System with a small servo motor mounted to the top of the frame. |
B-D) Our laboratory utilizes cutting edge technologies to develop customizable solutions at the prototyping stage. In a prior project, craniofacial scans with a Structure sensor were used to generate custom 3-D printed frames. |
D features a close up of a research subject wearing MLP glasses. |
|