The Clinical & Population Health Research (CPHR) doctoral program is one of the few in the country that was specifically designed to address the new challenges in biomedical research. These include speeding the translation of knowledge from the explosion in basic sciences to patient care interventions, and assuring that new evidence-based medicine reaches the populations that can benefit from it. The CPHR program promotes an interdisciplinary approach to conducting research, and provides a strong focus on addressing the needs of vulnerable populations.

Dr. Brown is an internationally known clinical researcher leading the quest to cure neurodegenerative and neuromuscular diseases like amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease. In 1993, a team of researchers led by Dr. Brown discovered the first gene linked to the inherited form of ALS, a protein anti-oxidant known as superoxide dismutase, or SOD1. Since the initial discovery of the SOD1 gene, Dr. Brown has played a major role in the discovery of other genetic mutations that cause or influence the survival time in ALS. His clinical research efforts focus on RNAi and gene-based therapies for familial cases of ALS stemming from the SOD1 mutations. In addition to his work with ALS, Dr. Brown has also identified disease genes in other inherited neurodegenerative and neuromuscular diseases such as hyperkalemic periodic paralysis, Miyoshi muscular dystrophy and hereditary sensory neuropathy.
Brown Lab


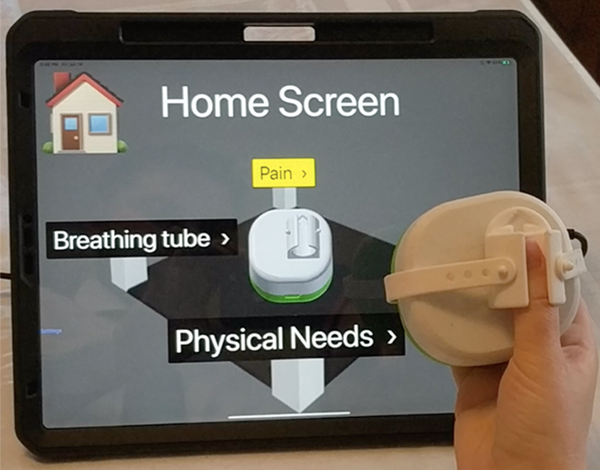
Dr. Walz is an attending anesthesiologist and Professor within the Department of Anesthesiology and Perioperative Medicine at the UMass Chan Medical School. Recently, he became chairperson of this department. As an investigator, he has distinguished himself as a leader in early, goal-directed mobilization of Surgical ICU patients, and he has conducted multiple studies of perioperative outcomes. He has completed multiple projects relating to anesthesia patient safety. Several of these deal with the prevention of infections related to surgery, others with the best management of catheters for anesthesia. Additionally, he has acquired expertise in critical care medicine, especially in relation to the prevention of infections in central venous catheters. Several of these have been large cohort studies. His familiarity in patient safety related to ICU activities and critical care medicine has informed his work in anesthesia patient safety.
matthias.walz@umassmemorial.org
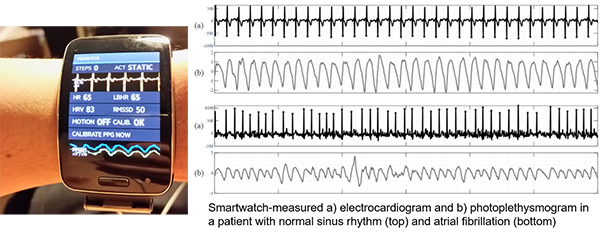

Dr. David McManus is a physician scientist whose work in cardiovascular science spans from translational and population health research to technical innovation and data science. His primary research aim is to better understand and manage patients with cardiovascular diseases using emerging mobile and digital technologies, with specific emphasis on atrial fibrillation. His lab employs a wide range of epidemiological, translational, behavioral, and machine learning methods to investigate different facets of applying digital solutions to cardiovascular healthcare.
david.mcmanus@umassmed.edu

Eric joined Dr. McManus’s lab in 2017, and his dissertation work focuses on streamlining the use and integration of smartwatches for atrial fibrillation detection into existing clinical infrastructures and frameworks. He is using a mixed-methods approaches and to amalgamate aspects of biomedical engineering, behavioral science, and clinical cardiology to ultimately improve rates of detection and quality of healthcare for older patients at risk for atrial fibrillation.
Eric.Ding@umassmed.edu
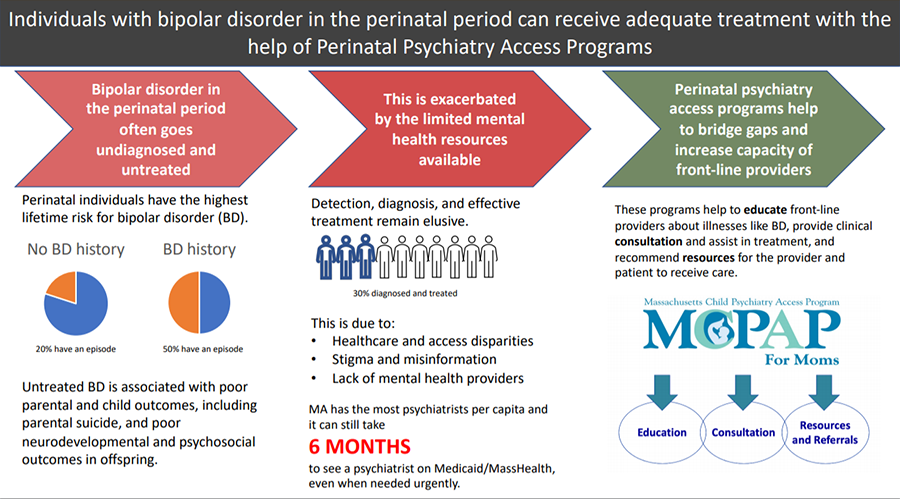

Dr. Byatt is a psychiatrist, physician-scientist, and perinatal mental health expert who is focused on improving health care systems to promote maternal mental health. She is an Associate Professor of Psychiatry and Ob/Gyn at the UMass Chan Medical School. She is the inaugural Medical Director of MCPAP for Moms, a statewide program that has impacted state and national policies regarding perinatal mental health and increased access to perinatal mental health care for thousands of women. Dr. Byatt has several federal grants that focus on developing and testing scalable interventions for addressing depression in obstetric settings. She frequently serves on national advisory boards and expert work groups focused on improving perinatal mental health. Her academic achievements have led to over 100 peer-reviewed publications, book chapters and national presentations and numerous national awards.
Research Lab

Bipolar disorder is a serious mental illness that affects pregnant and postpartum individuals disproportionately and is a significant cause of perinatal morbidity and mortality. Because bipolar disorder is hard to detect and treat in this population, these individuals often go without care, compounding illness risks. My dissertation aims to elucidate how to bridge gaps in care for pregnant and postpartum individuals with bipolar disorder and explore potential solutions, including that of better integration of obstetric and psychiatric care via Perinatal Psychiatry Access Programs.
Grace.Masters@umassmed.edu

Peter D. Friedmann, MD, MPH, DFASAM, FACP, Chief Research Officer and Endowed Chair for Clinical Research at Baystate Health, Associate Dean for Research, and Professor of Medicine & Quantitative Health Sciences, UMass Chan, is an addiction medicine physician and researcher. Dr. Friedmann began a two-year term as President of the Massachusetts Society of Addiction Medicine
(MASAM) on May 17, 2019. He is a primary care internist, addiction medicine clinician, & established substance abuse researcher who has published over 160 peer-reviewed articles on the organization of treatment services, treatment process & outcomes, implementation of evidence-based practices for substance use disorders (SUDs) in medical, specialty addiction and correctional settings and the role of the physicians in the care of patients with SUDs. He has had continuous funding from the National Institute on Drug Abuse (NIDA), National Institute on Alcohol Abuse and Alcoholism and Department of Veterans Affairs since 1996, and was a Robert Wood Johnson Generalist Physician Faculty Scholar. He is past president of the Association for Medical Education and Research in Substance Abuse (AMERSA), and former director on the American Board of Addiction Medicine.
Research Lab

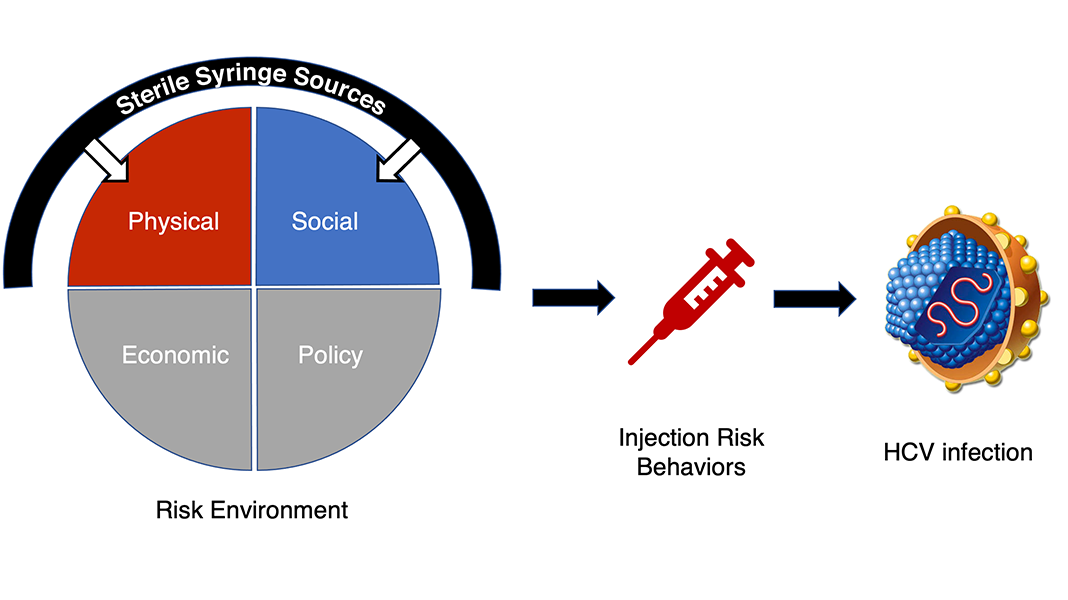
The ongoing opioid crisis has fueled an increase in injection drug use and a surge in new hepatitis C virus (HCV) infections that has disproportionately affected rural people who inject drugs (PWID). Although research has shown that syringe services programs are associated with a reduction in injection risk behaviors and HIV transmission, the evidence for whether these services reduce HCV risk among PWID remains mixed. My dissertation applies the risk environment model to investigate whether syringe services programs lower HCV risk by influencing the local physical and social environment. I am using mixed methods to (1) evaluate whether spatial proximity to syringe services programs and secondary syringe exchange are associated with HCV serostatus among rural PWID, and (2) explore PWID’s perceptions and experiences with obtaining syringes and syringe sharing practices.
Eric.Romo@umassmed.edu

Dr. Christine Ulbricht, PhD, MPH, is a psychiatric epidemiologist with expertise in advanced quantitative methods and mental health services research. Her current work focuses on examining the epidemiology of psychiatric disorders and related conditions among vulnerable populations in health service settings, such as nursing homes.
Research Lab

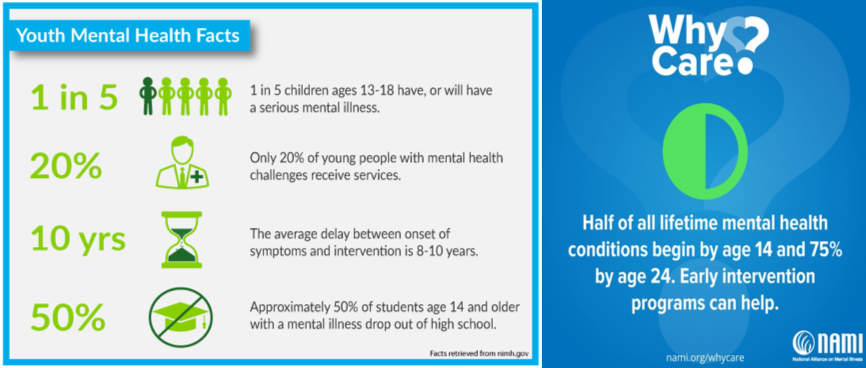
Julie began working with Dr. Christine Ulbricht in 2017. Since then, she has worked with the group to better understand working-age adults (22-64 years) living in nursing homes, many of whom have mental illness. Julie is interested in improving the lives of those living with mental illness, specifically through providing more equitable access to and improved quality of healthcare. Her dissertation work focuses on healthcare utilization of transition-age (16-25 years) youth with serious mental illness.
Julie.Hugunin@umassmed.edu

Arlene Ash is a PhD-level mathematician who has worked in medical schools as a health services research methodologist since 1984. Her areas of special interest and expertise include: design of experiments, building and validating models for predicting health care costs, utilization and other health outcomes in populations, comparing quality outcomes across providers, and conducting research into the causes and correlates of health disparities. She writes and lectures about a wide range of methods issues in study design, analysis and reporting, and has frequently led studies to evaluate the relative contributions to health outcomes of individual medical and social risks, medical interventions, and system-level factors.
Arlene Ash Lab

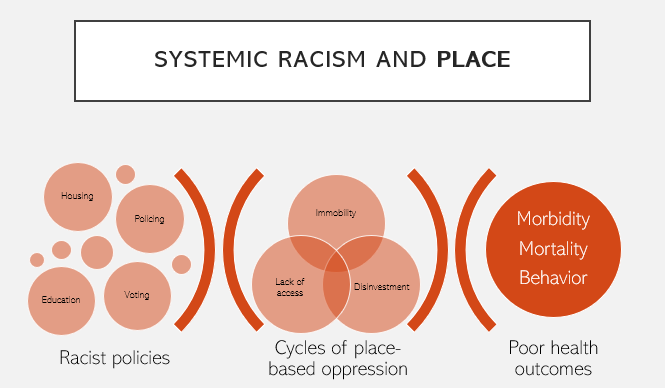
Despite huge investment in addressing inequities, structural racism, what many recognize as the root cause for unequal mortality and burden of disease, is poorly quantified with current measures. My research aims to characterize the health impact of historic structural racism through the validation of an improved composite measure of publicly available data on neighborhood-level social determinants of health.
Zachary.Dyer1@umassmed.edu Research Lab

Jay Himmelstein M.D., MPH, is a Professor of Population and Quantitative Health Sciences and Family Medicine and Community Health, and Chief Health Policy Strategist for ForHealth Consulting at the UMass Chan Medical School. His professional career in research, policy development, and service has been dedicated to improving health care and health outcomes for those served by the public sector. He has placed special emphasis on Medicaid programs and health services for people with disabilities, and is a nationally recognized physician, educator and researcher. Dr. Himmelstein’s most recent work has focused on the intersection of health policy and information technology, improving coordination of care and transitioning from fee-for-service to value-based payments in Medicaid programs, and leveraging University partnerships with Medicaid agencies to facilitate health system transformation.
Himmelstein Lab