The Brehm and Greiner Labs Tested a Lockheed Martin Developed Pancreatic Islet Encapsulation Device
Date Posted: Thursday, September 05, 2019
The research laboratories of Dale Greiner, PhD and Michael Brehm, PhD at the UMass Chan Diabetes Center of Excellence (DCOE) collaborated with JDRF Research and Lockheed Martin on novel technology developed by Lockheed Martin for the purpose of pancreatic islet encapsulation.
Encapsulation is defined as the transplantation of insulin-producing beta cells that are protected by and contained within a capsule. The ideal encapsulation device would protect the cells from the type 1 diabetes autoimmune attack, while also allowing those protected cells to survive and function.
Challenges of Islet Encapsulation
Three major obstacles to pancreatic islet encapsulation have presented problems to scientists over the years.
1. Cell Supply
The only proven source of donated islet cells to date have come from cadavers, of which the supply is extremely limited.
2. Cell Health and Survival
Islets require oxygen to survive. A successful encapsulation device must support artery and tissue growth, allowing oxygen to be carried into the device and to the cells. That would enable the beta cells to release insulin into the blood.
3. Protection from the Body’s Immune Response
Scarring around the device, known as fibrosis, is caused when the body's immune system recognizes the encapsulation device in the body and attacks it. Fibrosis has been the most common reason that past encapsulation devices have not been successful.


Encapsulation Device Optimization
The Greiner and Brehm labs at the UMass Chan DCOE tested Lockheed Martin’s encapsulation device. Their engineers were working to optimize the application of graphene, a one atom thick material, in the design of novel encapsulation devices for islets. Those graphene sheets were intended to generate encapsulation devices to protect islets from immune rejection while also allowing a highly permeable barrier that enables instantaneous diffusion of glucose, insulin, oxygen and nutrients to and from the islets.
“The technological advances being made at Lockheed are an exciting step forward for islet transplantation and the treatment of diabetes,” said Dr. Brehm in 2019 as the experiments were taking place. “Moreover, as the technology matures, it may have broad application in areas of clinical therapy.”
JDRF’s encapsulation research program funded the collaborative research to overcome the barriers and create a successful implantable cell replacement device to be used as a therapy for people living with type 1 diabetes.
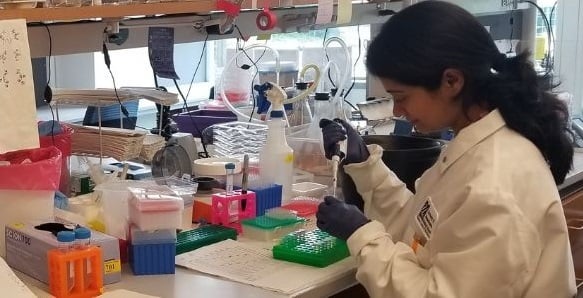
Shantashri Vaidya, PhD, led the islet encapsulation study in the Brehm Lab
