
Multiple Sclerosis is an inflammatory disease of the central nervous system caused by an abnormal immune system response. It commonly manifests with recurrent episodes of new neurological deficits over an hours- or days-long time scale. These flares are associated with injury to the brain and spinal cord; this tissue damage can be visualized using MRI scans. Many people with MS will even accumulate smaller, injurious lesions between flares, often without realizing. Left untreated, MS can lead to the irreversible accumulation of neurological problems.
Fortunately, the field has made tremendous advances in treatment over the past several decades. Contemporary medicines are extremely effective at halting the appearance of new "inflammatory" injury in the brain and spinal cord, and halting clinical relapses. Amazingly, all of this progress has occurred without a true understanding of the disease mechanisms. One "surprising" breakthough that occurred in the past couple of decades was the success of a therapy that depletes the B-cells of the immune system. Prior to this, the disease was recognized to be mostly a T-cell mediated process (both are true).
Some of the latest research points toward the Epstein-Barr Virus as an early causative agent. In an unlucky minority, this virus (that has infected >90% of the adult population) seems to associated with — or initiates — an immune response that leads to MS. It remains unclear why it takes about 10 years from the time of infection to the onset of MS symptoms.
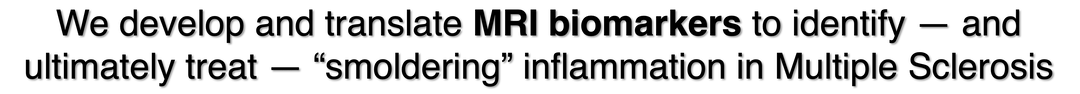
In the context of these incredible therapeutic successes, the clinical focus on MS has turned toward the more insidious aspects of the disease. Some people with MS will experience slow worsening of their neurological function, even in the complete absence of new MRI-visible lesions in their brain or spinal cord. This "smoldering" disease is more difficult to identify and treat. But without good biomarkers to measure this process, developing new medications remains extremely challenging. The identification and developmental translation of imaging biomarkers is one of the primary focuses of the Hemond lab. The paramagnetic ("iron") rim lesion (PRL) is one excellent example of a candidate imaging marker. However, it may not capture the breadth of processes that are involved in the "smoldering" inflammatory process, and this clinical gap remains one of the most important areas for ongoing research.