Wednesday, August 15, 2018
|
............................................................................................................................................................................................
→ Dan Mullin, Director of the UMass Center for Integrated Primary Care discusses a recently published article about MAT in primary care and reflects on what CIPC has been doing in this regard.
............................................................................................................................................................................................
The opioid epidemic continues to inflict a significant human and financial cost in the United States. A July article in the New England Journal of Medicine by Drs. Sarah Wakeman and Michael Barnett provides a helpful summary of the myths and realities associated with buprenorphine (Suboxone) and the opioid epidemic.
Primary Care and the Opioid-Overdose Crisis - Buprenorphine Myths and Realities. Wakeman, S. E., & Barnett, M. L. (2018). Primary Care and the Opioid-Overdose Crisis - Buprenorphine Myths and Realities. The New England Journal of Medicine, 379(1), 1–4. https://www.nejm.org/doi/10.1056/NEJMp1802741
This systematic and thoughtful examination of prevailing or unhelpful attitudes towards addressing OUD in primary care offers hope for stemming and controlling OUD.
Addressing OUD in primary care—possible? Or not?
The authors list a number of myths regarding buprenorphine including:
“The first myth is that buprenorphine is more dangerous than other interventions physicians master during training.”
“The second myth is that buprenorphine is simply a “replacement” and that patients become “addicted” to it — a belief still held by some physicians. But addiction is defined not by physiological dependence but by compulsive use of a drug despite harm. If relying on a daily medication to maintain health were addiction, then most patients with chronic health conditions such as diabetes or asthma would be considered addicted.”
“A closely related myth is that abstinence-based treatment, usually implying short-term detoxification and rehabilitation, is more effective than medication for addiction treatment.” and “…no study has shown that detoxification or 30-day rehabilitation programs are effective at treating opioid use disorder.”
And finally, the authors point out that, “some observers believe that physicians should simply stop prescribing so many opioids. The crisis began with increased opioid prescribing, yet as prescribing rates have fallen since 2011, overdose deaths have accelerated.”
I urge you to read the article as it provides the evidence to demolish the myths and bring readers to a more accurate reality. PCPs can successfully treat opioid use disorder in their primary care practices, and in community health centers. Behavioral health providers can assist them with this important work. The US healthcare system has experience in managing populations with chronic diseases such as diabetes, asthma, and HIV in primary care, and we can do the same with OUD.
UMass CIPC plays an active role in the reality of combating OUD
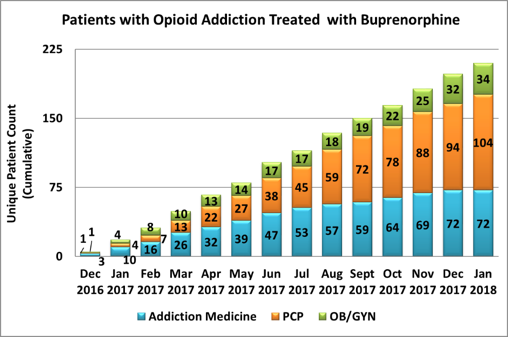
The UMass Center for Integrated Primary Care continues to play an active role in training primary care teams to respond to the needs of patients with Opioid Use Disorder. These efforts have included:
- Operating a Project ECHO Hub providing live, weekly, case-based learning to PCPs prescribing buprenorphine. In 2017, Bassett Healthcare Network in New York contracted with the CIPC to deliver MAT focused trainings to their providers. Bassett Healthcare Network successfully expanded MAT across the primary care network as part of their Delivery System Reform Incentive Payment contract. As a result of the CIPC’s trainings, the Healthcare Association of New York State awarded Bassett one of four 2018 Pinnacle Awards for Quality and Patient Safety for its addiction treatment program. https://www.hanys.org/news/?storyid=5264
- Applying for federal funding from the Substance Abuse and Mental Health Services Administration to build and implement buprenorphine waiver training in all 4 of Massachusetts Medical Schools (Tufts, Harvard, Boston University, and the University of Massachusetts).
- Building a patient and family, interactive, educational website focused on increasing awareness of the safety and efficacy of buprenorphine treatment. This project was made possible by a grant from the Blue Cross Blue Shield Foundation of Massachusetts. The website is scheduled to go live in early 2019.
- Delivering buprenorphine waiver training to health systems and primary care associations, such as the Alaska Primary Care Association. In September of 2018 Drs. Mullin and Martin will travel to Sitka, Alaska to deliver 2 days of training on integrated care and Medication Assisted Training, including 8 hours of qualifying DEA-X waiver training for PCPs.