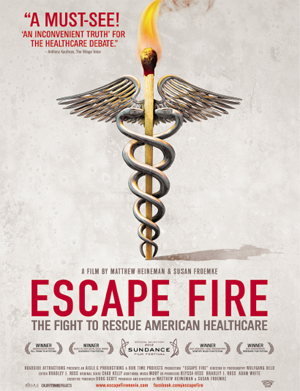
More than 350 people gathered in the three amphitheaters in the Medical School building for an advanced screening of the film Escape Fire: The Fight to Rescue American Healthcare on Tuesday, Sept. 19. UMMS was one of 50 medical schools participating in the screening, which was co-sponsored by the American Medical Student Association (AMSA), the Institute for Healthcare Improvement (IHI), Planetree Patient Relations and UMass Memorial Medical Center.
The title of the movie references a term that originated during a forest fire in Mann Gulch, Mont. In an effort to protect himself from an oncoming blaze, one man deliberately set fire to the area nearby, depleting what would have otherwise been fuel for the larger fire. As other men tried and failed to use conventional methods to save their own lives, this one resourceful and innovative firefighter was able to outlast the fire in the newly burnt area and emerge from the ordeal unharmed. Don Berwick, MD, former administrator of the Centers for Medicare and Medicaid Services, who is featured prominently in the film, draws a parallel between this story and America’s current health care crisis: “We’re in Mann Gulch. Health care, it’s in really bad trouble. The answer is among us. Can we please stop and think and make sense of the situation and get our way out of it?”
The movie highlights the innumerable ways in which the fires of the health care crisis are looming, offering some staggering statistics to support its claims. According to the move, the root of the problem is the fact that Washington, Wall Street and medicine are all inextricably linked. The power of marketing and the pharmaceutical-centered mindset of physicians and patients alike has led to the United States spending $300 billion on pharmaceuticals annually—almost as much as the rest of the world combined. In 2010, $1.1 billion was spent on health care lobbying in Washington, underscoring the significant financial stake in health policy and the gargantuan effort it will take to rebuild our entrenched system.
A key theme in the film is our country’s lack of focus on preventative care—more than 75 percent of health care costs go to treating preventable diseases. Physicians have more knowledge about what can be done to make patients better than what can be done to help them stay better. Andrew Weil, MD, founder of the University of Arizona Center for Integrative Medicine, argues “we don’t have a health care system in this country, we have a disease management system.”
Escape Fire advocates for a shift from our current disease-based approach to a focus on treating the whole person. The Preventative Medicine Institute founded by Dean Ornish, MD, receives considerable attention in the film as a model of how a healthy lifestyle could not only control, but reverse coronary artery disease. Even the U.S. military has started to incorporate acupuncture, yoga and meditation into the treatment of veterans who rely on opiates and anti-depressants to deal with the physical and emotional trauma of war. Incorporation of these lifestyle changes into mainstream health care as a complement, or even replacement, for Western medicine could both lower health care spending and improve quality of life.
More important than the movie were the discussions and emotions that it engendered. The panel after the screening consisted of a diverse group of participants, ranging from students to patients to administrators at both the hospital and medical school level. Each panelist gave his own reactions to the film. Robert Klugman, MD, associate professor of medicine, who is both the UMass Memorial Medical Center chief quality officer and a primary care doctor himself, echoed the sense of loneliness physicians felt in the film, citing the pressures of payers, government and the pharmaceutical industry as reasons for such feelings.
Although the task of changing the American health care system is daunting, there was an air of energy and determination in the room. Melissa Fischer, MD, associate professor of medicine and associate dean for undergraduate medical education, commented on the energy and activism within the UMMS–UMass Memorial community and encouraged its continuation. Dan Wolpert, panelist and member of the UMass Memorial Medical Center Patient and Family Advisory Council, emphasized the importance of patients continuing to advocate for their own rights. Indeed, the passion of both providers and patients is needed to present a united front in the effort to fix a broken system.
With the upcoming elections and considerable uncertainty about the future direction of health care, it is important to continue to have these dialogues and to carry this energy forward; such momentum can help our nation break free of our unsustainable model and attain a better system. It will take considerable effort to change, but continuing the status quo is impractical. In the words of Stephen Martin, MD, assistant professor of family medicine & community health and faculty organizer of the event, “We didn’t leave the Stone Age because we ran out of stones.”